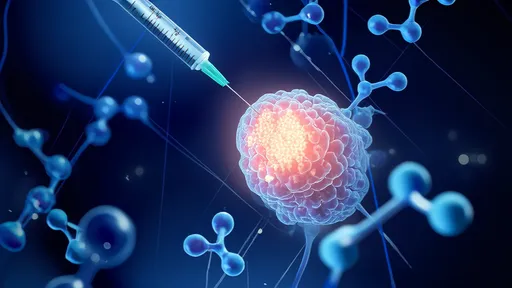
The scientific community is abuzz with cautious optimism as researchers explore a groundbreaking approach to treating Parkinson's disease—mitochondrial injection therapy. This innovative strategy targets the very power plants of our cells, aiming to reverse the energy deficits that characterize this debilitating neurodegenerative disorder. Unlike traditional treatments that merely manage symptoms, this therapy attempts to address the root cause of cellular dysfunction in Parkinson's patients.
At the heart of this experimental treatment lies a simple yet profound biological truth: healthy mitochondria are essential for neuronal survival. These tiny organelles serve as cellular batteries, generating the adenosine triphosphate (ATP) that fuels every thought, movement, and biological process. In Parkinson's disease, dopamine-producing neurons in the substantia nigra gradually deteriorate, and their mitochondria appear particularly vulnerable to damage. The resulting energy crisis within these cells triggers a cascade of dysfunction that ultimately leads to their demise.
The therapy involves extracting healthy mitochondria from a patient's own cells—typically from muscle tissue or platelets—and injecting them directly into affected brain regions. This autologous approach minimizes rejection risks while providing compromised neurons with fresh, functional mitochondria. Early-stage clinical trials have shown that these transplanted mitochondria can integrate with host cells, potentially restoring energy production and slowing neurodegeneration.
Breaking the Cycle of Cellular Exhaustion
What makes mitochondrial injection particularly promising for Parkinson's is its potential to interrupt the vicious cycle of oxidative stress and energy depletion. Diseased mitochondria leak reactive oxygen species that damage cellular components, including the mitochondria themselves. By introducing healthy organelles, researchers hope to break this destructive feedback loop. The therapy appears to not only boost ATP production but also improve calcium buffering and reduce oxidative stress—all critical factors in neuronal survival.
Recent animal studies have yielded remarkable results. In primate models of Parkinson's, mitochondrial transplantation led to measurable improvements in motor function and delayed disease progression. Post-mortem examinations revealed that treated animals preserved significantly more dopamine neurons compared to controls. Perhaps most intriguingly, the benefits appeared to extend beyond simple energy support, suggesting the transplanted mitochondria may be triggering broader neuroprotective mechanisms.
The human trials conducted so far have been small in scale but encouraging. In one pilot study, patients receiving mitochondrial injections alongside standard medication showed improved motor scores and reduced medication requirements. Functional MRI scans revealed increased activity in previously quiescent brain regions, hinting at possible neural network reorganization. While these findings require replication in larger cohorts, they suggest we may be witnessing the dawn of a new therapeutic paradigm.
Technical Challenges and Ethical Considerations
Despite its promise, mitochondrial injection therapy faces significant hurdles. Delivering these organelles precisely to affected brain regions requires sophisticated neurosurgical techniques. The blood-brain barrier presents another obstacle, though researchers are developing specialized delivery methods to circumvent this protection. There are also questions about the longevity of transplanted mitochondria and whether repeated treatments might be necessary.
Ethical discussions have emerged regarding the source of mitochondria. While using a patient's own tissue is currently standard, some scientists speculate about the potential benefits of using mitochondria from younger donors or stem cell-derived organelles. This raises complex questions about cellular therapies that the medical community must address as the technology advances.
The financial aspect cannot be ignored either. As a highly personalized, labor-intensive therapy, mitochondrial transplantation would likely carry substantial costs. Researchers are working to streamline the mitochondrial isolation and preparation processes to make the treatment more accessible if it proves effective in larger trials.
The Road Ahead for Parkinson's Treatment
As the scientific community awaits results from ongoing clinical trials, mitochondrial injection therapy represents one of the most biologically plausible approaches to modifying Parkinson's disease progression. Unlike many experimental treatments that show promise in animals but fail in humans, this approach builds upon well-established principles of cellular energetics. The therapy's potential synergy with existing treatments—possibly allowing lower doses of levodopa with reduced side effects—adds to its appeal.
Long-term questions remain about how long the benefits might last and whether the treatment could prevent disease progression if administered early enough. Researchers are particularly interested in exploring whether mitochondrial therapy could benefit patients with genetic forms of Parkinson's linked to mitochondrial dysfunction.
For now, cautious optimism prevails in the research community. While mitochondrial injection therapy won't be widely available for several years, its development marks an important shift from symptom management to cellular repair in neurodegenerative disease treatment. As one neuroscientist involved in the research noted, "We're not just putting bandages on damaged neurons—we're trying to give them the tools to heal themselves."
The coming years will be critical for determining whether this cellular energy reboot can deliver on its early promise. For millions living with Parkinson's disease and their families, the possibility of a therapy that addresses the underlying biology rather than just the symptoms offers a glimmer of hope in their long battle against this relentless condition.
By /Jul 18, 2025

By /Jul 18, 2025

By /Jul 18, 2025

By /Jul 18, 2025
By /Jul 18, 2025
By /Jul 18, 2025
By /Jul 18, 2025
By /Jul 18, 2025

By /Jul 18, 2025
By /Jul 18, 2025

By /Jul 18, 2025
By /Jul 18, 2025

By /Jul 18, 2025

By /Jul 18, 2025

By /Jul 18, 2025

By /Jul 18, 2025
By /Jul 18, 2025

By /Jul 18, 2025