The vagus nerve, a meandering superhighway of neural communication between brain and body, has emerged as an unexpected ally in the fight against chronic inflammation. Once viewed primarily as a regulator of heart rate and digestion, this cranial nerve is now at the center of groundbreaking bioelectronic medicine research. Scientists are mapping its intricate branches with unprecedented precision, revealing how targeted electrical stimulation might reboot the immune system—offering hope for millions suffering from inflammatory conditions resistant to conventional therapies.
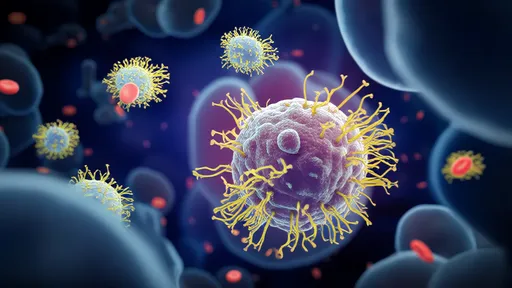
The Vagus-Immune Connection: Nature’s Built-In Anti-Inflammatory Circuit
What makes the vagus nerve uniquely suited for inflammation control is its direct line to the spleen, the immune system’s command center. When activated, certain vagal fibers trigger specialized T-cells that produce acetylcholine—a neurotransmitter that puts the brakes on overactive macrophages. This "inflammatory reflex" acts like a biological circuit breaker, preventing the cytokine storms that drive conditions from rheumatoid arthritis to Crohn’s disease. Recent studies using optogenetics have pinpointed exact neural pathways in animal models, showing how millisecond-precision stimulation can reduce TNF-alpha levels by 75% without immunosuppressive side effects.
Electrode Innovations: From Crude Pacemakers to Microscopic Neural Sculptors
The crude vagus nerve stimulators of the 1990s, originally designed for epilepsy, bear little resemblance to today’s third-generation devices. Flexible mesh electrodes now wrap around microscopic nerve bundles like ivy on a trellis, delivering current to specific fiber types (myelinated vs. unmyelinated) with sub-millimeter accuracy. Boston-based SetPoint Medical recently debuted a device that combines ultrasound guidance with AI-driven stimulation patterns, adapting in real-time to changes in inflammatory biomarkers. Meanwhile, researchers at the Feinstein Institutes have developed "neurograins"—rice-sized implants that modulate individual vagal branches controlling distinct organs.
Clinical Breakthroughs: Beyond Rheumatology
While early trials focused on rheumatoid arthritis (showing 50% symptom reduction in treatment-resistant cases), the therapeutic horizon has expanded dramatically. A 2023 multi-center study demonstrated vagal stimulation’s efficacy in reducing neuroinflammation in Alzheimer’s patients, slowing cognitive decline by 30% compared to controls. Even more striking are case reports of "inflammatory reset" in long COVID sufferers—patients with persistent fatigue and brain fog showed normalized cytokine profiles after just six weeks of targeted vagus nerve therapy. Gastroenterologists are now exploring transcutaneous vagal stimulation for ulcerative colitis, with preliminary data showing endoscopic improvement comparable to biologic drugs.
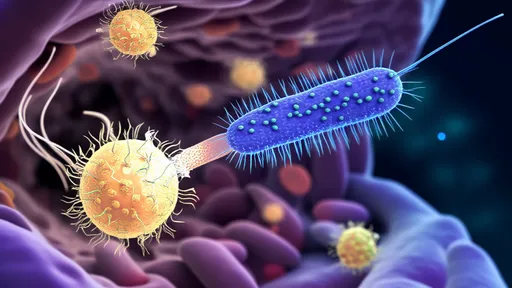
The Precision Challenge: Why One Stimulation Pattern Doesn’t Fit All
The vagus isn’t a simple on-off switch; its 160,000 fibers carry bidirectional traffic in a complex Morse code of neural signals. What works for a lupus patient might exacerbate symptoms in someone with psoriasis due to subtle differences in autonomic tone. Advanced computational models are helping decode these patterns—researchers at MIT recently published a "vagal alphabet" mapping how specific firing sequences activate different anti-inflammatory pathways. This explains why early, non-targeted stimulators yielded inconsistent results, and why personalized dosing protocols are revolutionizing outcomes.
The Future: Closed-Loop Bioelectronic Therapies
The next frontier involves implantable systems that continuously monitor inflammatory markers (via embedded biosensors) and adjust stimulation parameters autonomously. Galvani Bioelectronics, a GSK-backed startup, is testing a device that detects IL-6 spikes in real-time, delivering precisely timed pulses to counteract them. Such closed-loop systems could render weekly biologic injections obsolete for many patients. Meanwhile, non-invasive approaches like transcutaneous auricular vagus nerve stimulation (taVNS) are gaining traction, with smart earbuds that modulate inflammation during sleep showing promise in early trials.
As the vagus nerve’s intricate topography comes into sharper focus, bioelectronic medicine stands poised to disrupt the $100 billion global market for anti-inflammatory drugs. The convergence of neural mapping, materials science, and AI is transforming this ancient nerve into a dynamic therapeutic interface—one that harnesses the body’s innate wisdom rather than overriding it with pharmaceuticals. For patients weary of the side effects and diminishing returns of conventional treatments, this electrifying approach offers more than hope—it offers the potential for lasting remission written in the language of neural signals.
By /Jul 18, 2025

By /Jul 18, 2025

By /Jul 18, 2025

By /Jul 18, 2025
By /Jul 18, 2025
By /Jul 18, 2025
By /Jul 18, 2025
By /Jul 18, 2025

By /Jul 18, 2025
By /Jul 18, 2025

By /Jul 18, 2025
By /Jul 18, 2025

By /Jul 18, 2025

By /Jul 18, 2025

By /Jul 18, 2025

By /Jul 18, 2025
By /Jul 18, 2025

By /Jul 18, 2025